River Safety and Rescue (revisited)

After the first of the year I'll be running some Basic and Advanced Swiftwater Rescue Courses, hopefully some of you will join me for one of those. For now... Get a little of this stuff in your head. Then everyone get out and get BFA/CPR certification!
Some of you already know this stuff, others may have never seen it. The fact of the matter is that all of us should know this information. Whenever we take part in any high risk activity such as kayaking (face it, we can't breathe underwater) we should do all that we can to insure our safety and the safety of the others around us. The strongest plan of action is one of Preparation & Prevention. All paddlers should at the very least gain certification in BFA/CPR and take part in a Basic SWR course. Though I would recommend a WFR course and an Advanced SWR course for anyone running serious class IV-V whitewater on a regular basis, especially people doing wilderness runs. Trust me, you want to be amply trained / equipped to deal with the unforeseen problems when they arise.

First Aid Tips
BEING TRAINED IN BASIC FIRST AID AND CPR IS CRITICAL IN SAVING LIVES DURING AN EMERGENCY!
- Stay calm
- Restore breathing and circulation
- Stop bleeding: Apply direct pressure to the wound and elevate it.
Prevent Shock:
- Lay victim on his/her back. Position the head below the feet. Monitor breathing and circulation. Do not move people with neck or spinal injuries unless it is necessary to establish or maintain vital A-B-Cs.
Chest Pain:
- Keep the conscious victim in a comfortable position with the head raised. Loosen tight clothing.
- Help victim take prescribed medications if necessary.
- If the victim loses consciousness and is not breathing, proceed with A-B-C's of rescue breathing. If there is no pulse, begin CPR if you are trained to do so.
When possible call 9-1-1 before starting A-B-Cs. Remember to give your location, the facts and stay on the line until the operator tells you to hang up.
IT’S AS EASY AS A-B-C
A-AIRWAY, B-BREATHING, C-CIRCULATION…
A-AIRWAY
- Place victim flat on his/her back on a hard surface.
- Gently shake victim at the shoulders and shout, “are you okay?”
- Head-tilt/chin-lift – open victim’s airway by tilting their head back with one hand while lifting up their chin with your hand.
B-BREATHING
- Position your cheek close to the victim’s nose and mouth, look toward victim’s chest; AND
- Look, listen, and feel for breathing (5-10 seconds).
- If not breathing, pinch victim’s nose closed and give a full breath into the victim’s mouth (use a micro shield).
- If breaths won’t go in reposition the head and try again to give breaths. If still blocked, perform abdominal thrusts (Heimlich maneuver).
If the person is unconscious;
- Check for pulse by feeling for 5-10 seconds at the side of victim’s neck.
- If there is a pulse, but the victim is not breathing, give Rescue breathing. Take a normal (not a deep) breath before giving rescue breath to victim. Give each breath over one second. Each breath should make the chest rise.
- If there is no pulse, begin chest compressions as follows: Place heel of one hand on lower part of victim’s sternum. With your other hand directly on top of first hand depress sternum 1.5-2 inches.
- Allow chest to recoil (return to normal position) completely after each compression, and use approximately equal compression and relaxation times. Try to limit interruptions in chest compressions. Every time you stop chest compressions, blood flow stops.
- Check for return of pulse every minute.
Note: It is highly recommended that persons be properly trained to perform CPR.

Casualty Assessment
What’s decided on in the first moments of an emergency could make all the difference!
APPROACH
Introduce Yourself.
Introduce yourself as a rescuer while moving toward the victim. This helps to alleviate anxiety and establishes your authority. You may also learn something about the victim's level of consciousness by their reaction to you.
Warn The Victim To Be Still.
Warn the victim to be still (not to move his head if a trauma to the head/spine may have occurred) and calm. The victim will be more responsive to a calm and professional approach.
Level Of Consciousness.
You must now determine the victim's general level of consciousness (A.V.P.U.). While approaching the victim, talk to him loudly and clearly to determine if there is any response to verbal stimulus. If the patient does not respond to your voice, quickly check for any response to painful stimulus by pinching the earlobe and/or rubbing the sternum with your knuckles (preferred).
A - Alert. Is the victim alert?
V - Verbal. Does the victim respond to questions?
P - Painful. Does the victim respond to painful stimulus?
U - Unresponsive. Is the victim completely unresponsive?
PRIMARY ASSESSMENT

Assess and treat the following priorities in order. Do not skip any priority.
Cervical Spine.
If the victim has suffered a trauma, which may have injured the cervical spine, you must provide support MANUALLY (using knees and hands) while you continue with the primary assessment. Do not move the victim or allow the patient to move on his own without providing support. Do not move a victim with a suspected spinal injury in order to treat or assess conditions not covered by the primary assessment or to take vital signs. If you MUST move a victim to assess or treat the ABCs, first bring the head to an anatomically neutral position while applying slight traction. Make sure the victim's body is immobile while this is being done. Once the head is in the neutral position, carefully move the victim to a stable position. A rigid collar should now be applied A.S.A.P. providing this does not significantly delay assessing the ABCs. MANUAL SUPPORT MUST BE MAINTAINED AT ALL TIMES.
Airway.
Is the airway patent (open)? Does the victim need to be repositioned or suctioned? If the victim is unresponsive, use the Modified Jaw Thrust (trauma incident) or Head Tilt - Chin Lift (medical) to ensure an open airway in order to assess whether the patient is breathing. If the patient is unresponsive and is positioned so that the tongue may possibly obstruct the airway, insert a mechanical airway.
Breathing.
Is the victim breathing on his own? If the victim is not breathing give two ventilations then check the pulse.
Circulation.
Can you find a carotid pulse? Are chest compressions necessary?
Bleeding /Wet Check.
Do a quick thorough head to toe physical and visual examination to determine if there is any bleeding taking place that would be considered life threatening.
Blanket And Oxygen.
If there are any indications of respiratory distress, head injury or shock. Indications of respiratory distress include gasping, wheezing, HYPOventilation, HYPERventilation, flaring of the nostrils, cyanosis, pallor, chest pain, jugular vein distention, tracheal deviation and paradoxical movement upon breathing. Cover victim with a blanket, plan to evacuate to EMS (Administer oxygen).
You have now completed the examination for life-threatening problems. Cover the victim if you think it is appropriate.
Priorities may be treated concurrently if necessary. For example, an arterial bleed could be treated while breathing is being assessed but breathing assessment should not be delayed more than momentarily.
It must be remembered that you may never get past the primary assessment in some patients. A common example would be a V.S.A. victim. However, if you do get past the primary assessment you must remember to continually monitor the ABCs and the victim's level of consciousness.
CHIEF COMPLAINT/VITAL SIGNS
Now is a good time to get a set of vital signs. While the vital signs are being taken, begin investigating the cause of the Chief Complaint (the main thing that is wrong with the victim). Provide treatment if possible.
If the victim is conscious:
Ask the victim what is bothering him if you haven't already. He may be able to tell you the exact nature of of his problem. If pain is his Chief Complaint, try to learn more by asking him to describe it as fully as possible. PQRST can be used to help you focus on the cause of the pain.
P - Provoked. How did the pain start?
Q - Quality. What does the pain feel like? (eg. sharp stabbing?,dull ache? etc.
R - Region. Where is the pain located?
S - Severity. How bad does it hurt?
T - Time. When did the pain begin? Does it come and go? How frequently?
If the victim is unresponsive:
Always check for a Medic Alert bracelet. Bystanders and/or family may be able to help you discover the cause of the unconsciousness. Common causes of unconsciousness are listed below.
A - allergies or alcohol E - epilepsy I - insulin O - overdose U - uremia
T - trauma I - infection P - psychiatric reasons S - stroke or syncopy

For all victims, try to obtain answers to the questions contained in AMPLE. Record the information in a S.O.A.P. Report.
A - Allergies. Does the patient have any allergies to medications?
M - Medications. Is the victim taking any medications? If so, what are they? Where does he keep them? Has he taken any recently? When and how many? Were they effective?
P - Past Medical History. Does the victim have any history of medical problems that may be relevant to the current problem?
L - Last Ate. When did he last eat?
E - Event. How did the current problem develop?
As long as you maintain the ABCs and monitor the victim's level of consciousness it is not crucial that you discover the cause of the Chief Complaint.
SECONDARY ASSESSMENT
For non-trauma victims the secondary assessment is of lesser importance and not normally done.
For trauma victims, begin a systematic examination for further injuries. Serious injuries to the head, neck, spine, chest, abdomen, pelvis or femurs are potentially life-threatening and transportation to the hospital A.S.A.P. is of primary importance. Immobilize any suspected fractures and dress wounds if time permits.
The usual sequence is as follows:
NECK - Do not move the victim if you have any reason to suspect that a cervical injury may have occurred. If a rigid collar has not been applied, GENTLY feel the cervical spine looking for bumps, gaps, hot spots or deformities. Look for Jugular Vein Distention or Tracheal Deviation.
SKULL - Palpate the skull from front to back. Look for bleeding, bumps, bruises, depressions or patient reaction to pain.
EYES - Check for lacerations, foreign objects, pupillary size, equality and reaction to light. If the victim is conscious, check for normalacy of vision. Look for bruising around the eyes. (raccoon eyes) This is an indication of a possible skull fracture.
EARS - Check for fluid discharge, lacerations, lumps or bumps. Also check for bruising behind the ears. (battle signs) This is also an indication of a possible skull fracture.
NOSE - Check for lacerations, fluid discharge, patency, bruising or flaring of the nostrils. (an indication of respiratory distress)
MOUTH - Check for airway patency, (eg. vomitus, food, dentures, blood) swelling, bruising, lacerations, pain on biting, alignment of the jaw and odors.
FACE - Check for lacerations, bruising, deformity color and temperature.
SPINE - GENTLY feel the remainder of the spine looking for bumps, gaps, hot spots or deformities. DO NOT MOVE THE VICTIM TO CARRY OUT THIS ASSESSMENT.
CHEST - Check for symmetry, lacerations, bruising deformities and puncture wounds. (if you find an entry wound, look for an exit wound) Palpate for pain or deformities of clavicles or scapula. Check for pain on compression of the sternum and rib cage. Watch for paradoxical movement upon breathing.
ABDOMEN - Check for lacerations and bruising. Palpate all four quadrants of the abdomen. Look for hot spots, tenderness, distention, rebound pain or guarding.
PELVIS - Check for lacerations, bruising, deformities and tenderness. Check for pain on GENTLY stressing the pelvic girdle. Listen and feel for crepitus.
EXTREMITIES - Check for deformities, pain, swelling, lacerations, bruising, needle marks, bites, cyanosis, impairment of sensation, movement and strength. Compare left and right sides.
TRANSPORT
Once EMS personnel arrive they will assume authority for the victim. You should make a complete report to them of the victim's condition and of all treatments you have given. Give them a copy of your S.O.A.P. Report.

Head injury
Alternative names
Concussion - first aid; Brain injury; Head trauma
Definition.
A head injury is any trauma that leads to injury of the scalp, skull, or brain. These injuries can range from a minor bump on the skull to a devastating brain injury.

Head injury can be classified as either closed or penetrating. In a closed head injury, the head sustains a blunt force by striking against an object. A concussion is a type of closed head injury that involves the brain.

In a penetrating head injury, an object breaks through the skull and enters the brain. (This object is usually moving at a high speed such as a kayaker running a large drop hitting rocks.)
Considerations.
Every year, millions of people sustain a head injury. Most of these injuries are minor because the skull provides the brain with considerable protection. The symptoms of minor head injuries usually go away on their own. More than half a million head injuries a year, however, are severe enough to require hospitalization.
Learning to recognize a serious head injury, and implementing basic first aid, can make the difference in saving someone's life.
In patients who have suffered a severe head injury, there is often one or more other organ systems injured. For example, a head injury is sometimes accompanied by a spinal injury.
Causes.
Accidents are the leading cause of death or disability in men under age 35, and over 70% of accidents involve head injuries and/or spinal cord injuries.
Common causes of head injury include traffic accidents, falls, physical assault, and accidents at home, work, outdoors, or while playing sports.
Some head injuries result in prolonged or non-reversible brain damage. This can occur as a result of bleeding inside the brain or forces that damage the brain directly.
These more serious head injuries may cause:
- Changes in personality, emotions, or mental abilities
- Speech and language problems
- Loss of sensation, hearing, vision, taste, or smell
- Seizures
- Paralysis
- Coma
Symptoms.
The signs of a head injury can occur immediately or develop slowly over several hours. Even if the skull is not fractured, the brain can bang against the inside of the skull and be bruised. (This is called a concussion.) The head may look fine, but complications could result from bleeding inside the skull.
When encountering a person who just had a head injury, try to find out what happened. If he or she cannot tell you, look for clues and ask witnesses. Look for a mechanism for injury. In any serious head trauma, always assume the spinal cord is also injured.
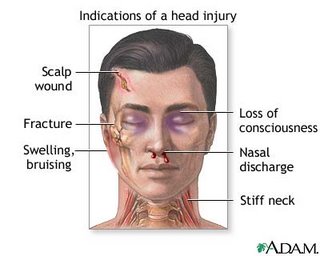
The following symptoms suggest a more serious head injury that requires emergency medical treatment:
- Loss of consciousness, confusion, or drowsiness
- Low breathing rate or drop in blood pressure
- Convulsions
- Fracture in the skull or face, facial bruising, swelling at the site of the injury, or scalp wound
- Fluid drainage from nose, mouth, or ears (may be clear or bloody)
- Severe headache
- Initial improvement followed by worsening symptoms
- Irritability (especially in children), personality changes, or unusual behavior
- Restlessness, clumsiness, lack of coordination
- Slurred speech or blurred vision
- Inability to move one or more limbs
- Stiff neck or vomiting
- Pupil changes
- Inability to hear, see, taste, or smell

First Aid.
Get medical help immediately if the person:
- Becomes unusually drowsy
- Develops a severe headache or stiff neck
- Vomits more than once
- Loses consciousness (even if brief)
- Behaves abnormally
For a moderate to severe head injury, take the following steps:
Call 911.
- Check the victim's airway, breathing, and circulation. If necessary, begin rescue breathing and CPR.
- If the victim's breathing and heart rate are normal but the victim is unconscious, treat as if there is a spinal injury. Stabilize the head and neck by placing your hands on both sides of the victim's head, keeping the head in line with the spine and preventing movement. Wait for medical help.
- Stop any bleeding by firmly pressing a clean cloth on the wound. If the injury is serious, be careful not to move the victim's head. If blood soaks through the cloth, DO NOT remove it. Place another cloth over the first one.
- If you suspect a skull fracture, DO NOT apply direct pressure to the bleeding site, and DO NOT remove any debris from the wound. Cover the wound with sterile gauze dressing.
- If the victim is vomiting, roll the head, neck, and body as one unit to prevent choking. This still protects the spine, which you must always assume is injured in the case of a head injury. (Children often vomit ONCE after a head injury. This may not be a problem, but call a doctor for further guidance.)
- Apply ice packs to swollen areas.
For a mild head injury, no specific treatment may be needed. However, closely watch the person for any concerning symptoms over the next 24 hours. The symptoms of a serious head injury can be delayed. While the victim is sleeping, wake him or her every 2 to 3 hours and ask simple questions to check alertness, such as "What is your name?"
Over-the-counter pain medicine (like acetaminophen or ibuprofen) may be used for a mild headache. DO NOT take aspirin, because it can increase the risk of bleeding.
Do Not.
- DO NOT wash a head wound that is deep or bleeding a lot.
- DO NOT remove any object sticking out of a wound.
- DO NOT move the person unless absolutely necessary.
- DO NOT shake the victim if he or she seems dazed.
- DO NOT remove a helmet if you suspect a serious head injury.
- DO NOT pick up a fallen child with any sign of head injury.
- DO NOT drink alcohol within 48 hours of a serious head injury.
Call immediately for emergency medical assistance if:
- There is severe head or facial bleeding.
- The victim is confused, drowsy, lethargic, or unconscious.
- The victim stops breathing.
- You suspect a serious head or neck injury or the victim develops any symptoms of a serious head injury.
Prevention
- Always use safety equipment during activities that could result in head injury.

The information contained on this website is intended to serve as a guide for those who may need to provide first aid. It is not intended to be a substitute for professional medical advice or training.
Peace,
JAH WILL


